Options for Addressing Botulism
Botulism, a rare but potentially fatal illness, can be transmitted through several routes. This article will explore the most common pathways of botulism transmission and the preventative measures that can be taken.
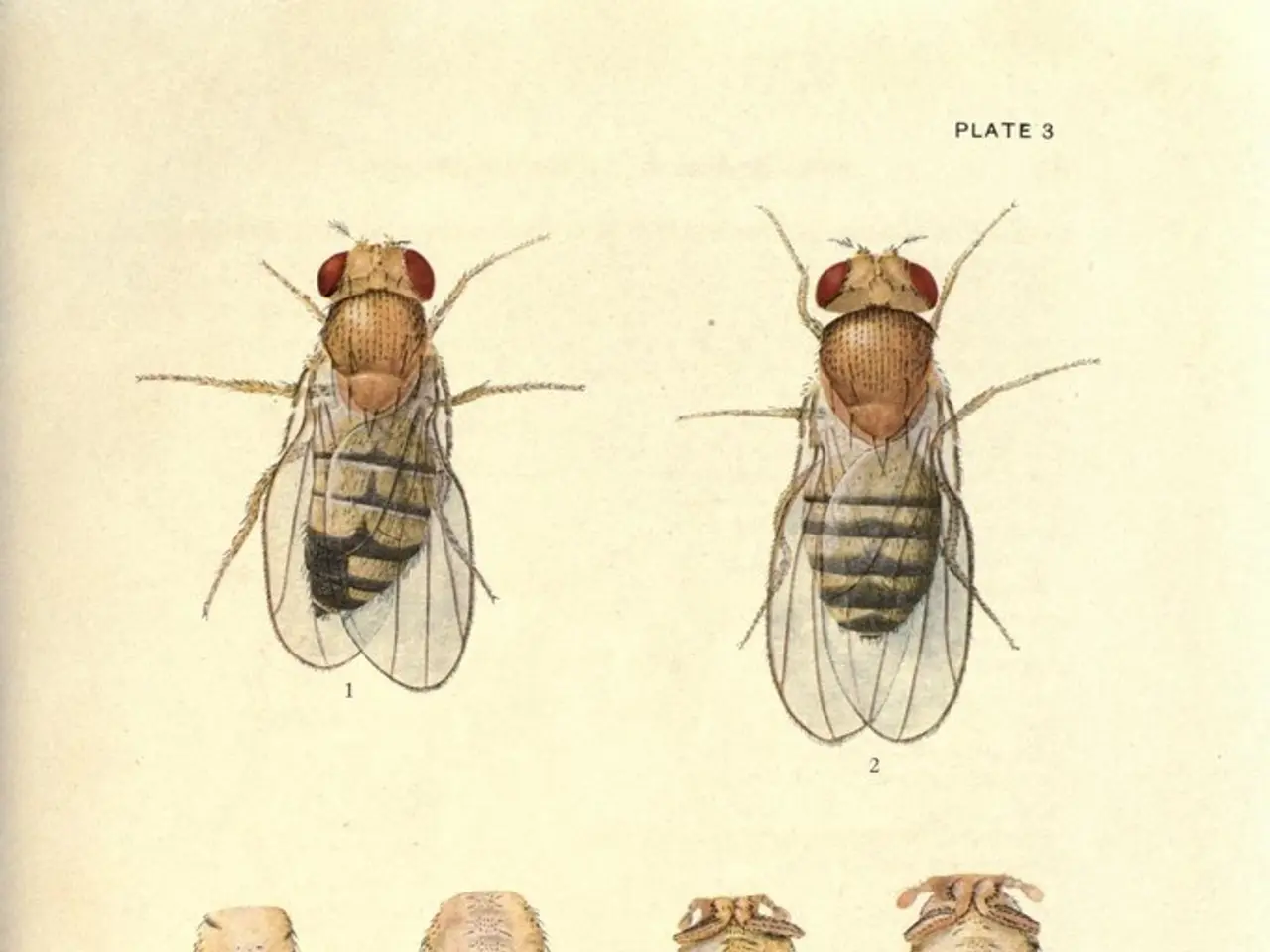
The bacterium responsible for botulism is Clostridium botulinum, a gram-positive, rod-shaped bacterium that thrives in anaerobic environments. There are eight strains of C. botulinum, each producing a different toxin.
One of the most common routes of transmission is foodborne botulism. This occurs when a person consumes food contaminated with C. botulinum spores or toxin. Common sources include improperly canned or preserved foods, where the bacteria grow and produce toxin. Home-canned foods are particularly notable sources, but commercially prepared foods can also be responsible if contaminated.
Wound botulism is another common route of transmission. This happens when C. botulinum spores infect a wound, germinate, and produce toxin locally. The bacteria enter through open wounds and generate toxin that leads to botulism symptoms.
Infant botulism, which affects children under 1 year old, occurs when they ingest spores that colonize their intestines and produce toxin in situ. Interestingly, C. botulinum can be found in honey and corn syrup for children under the age of 1, potentially leading to infant botulism.
Inhalational exposure to aerosolized botulinum toxin is recognized mainly in the context of bioterrorism or laboratory accidents, though it is less common than the above natural routes.
Preventative measures include proper cooking and preparation of canned food to inactivate C. botulinum. Laxatives, enemas, or other cathartics may be administered for foodborne botulism if there is no significant ileus. For wound botulism, antibiotics are administered alongside proper debridement, and the length of treatment varies based on the severity of the wound. However, antibiotics are not recommended for treating infant botulism or adults with suspected gastrointestinal botulism.
Diagnosis of botulism can be done through checking for signs of muscle weakness or paralysis, asking about food intake and exposure to the bacteria, and detecting the toxin in blood, gastric contents, or stool samples. Early diagnosis is crucial because paralysis can reach the respiratory muscles and cause difficulty in breathing.
It is essential to note that botulism is not contagious from human to human. Spores of C. botulinum exist in the environment, particularly in underground soil, rivers, and seawater.
In summary, the primary and most frequent transmission routes are ingestion of contaminated food (foodborne botulism), infection of wounds (wound botulism), and intestinal colonization in infants (infant botulism). Inhalational exposure is rare outside specific scenarios.
For more information on botulism, resources such as the Clinical guidelines for diagnosis and treatment of botulism (2021) and a systematic review and meta-analysis of cases from 1923 to 2016 are available.
The health-and-wellness sector should be aware that botulism, a neurological disorder, can be transmitted through various medical-conditions, such as foodborne botulism, wound botulism, and infant botulism. In the case of foodborne botulism, science indicates that consuming food contaminated with Clostridium botulinum spores or toxin is the primary cause, typically found in improperly canned or preserved foods. Wound botulism, on the other hand, results from C. botulinum infection of an open wound, leading to toxin production that causes symptoms. Infant botulism, which affects children under 1 year old, occurs when the spores colonize their intestines and produce toxin in situ, oftentimes through contact with contaminated food sources like honey or corn syrup. Preventative measures include proper food preparation, wound treatment, and avoidance of such contaminated sources. It's worth noting that botulism is not contagious from human to human.